The Roux-en-Y gastric bypass involves using a stapling device to completely separate the stomach into two compartments or pouches. A very small pouch is made immediately below the connection between the esophagus and the stomach. This leaves the vast majority of volume of the original stomach in the lower compartment. A portion of the mid small intestine is then attached to the upper, small pouch allowing for the passage of ingested material into the small intestine for absorption. Food and liquid that you swallow enters the upper, small compartment, but normally would never pass into the lower compartment (see illustration).
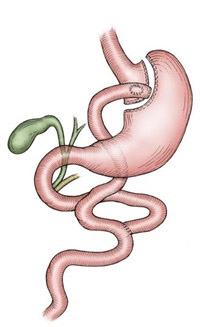
In gastric bypass surgery, surgical staples are used to divide the stomach and create a small upper pouch. The intestine is then divided and brought up to the small stomach pouch, bypassing the lower part of the stomach.
The small pouch serves as your new stomach, or reservoir, for food. As you eat, the food enters your pouch and is slowly emptied into your intestine. Because you have a very small stomach pouch, you will feel very full very quickly. Overeating can cause distention of the pouch, pain and vomiting. It can also potentially cause the staple line to disrupt or separate. Because of the small size of the pouch your eating habits will change drastically. You will never be able to eat the quantity of food you can currently eat. For example, most patients can eat about half a sandwich and a piece of fruit for lunch.
In addition to the effect on the size of your meals, the operation also results in nutrients bypassing the lower part of the stomach and the upper part of the small intestine. Although the percentage of nutrients that pass through into the stool without being absorbed is small, this does contribute to weight loss. In those patients with a BMI greater than 50, the bypassed segment of intestine is made slightly longer to help increase the amount of weight loss achieved.
Initially, after surgery, patients can only eat very small quantities of food, and the average daily intake is only 500-700 calories. Over time, the body adapts to the new anatomy, and caloric intake will rise to around 1200-1400 calories per day after one to two years. Although some of this increase is due to an increase in the size of the pouch (“stretching”), most is probably due to adaptation of the sensory nerves of the stomach and small intestine.
Although the principle of the gastric bypass is simple, it is a technically demanding procedure in the obese patient. Access to the abdominal cavity is gained through a single incision from just below the breastbone to the belly button. Since the middle 1990’s, certain centers have started performing the operation using a laparoscopic approach. This involves using five or six small incisions across the upper abdomen. A small telescope, thin instruments, and thin stapling devices are used to achieve the same anatomical result as with the open approach. Although the laparoscopic approach has appeal, it has not been proven to be safer or more effective than the open approach.
Early results show that the weight loss effects and decrease in co-morbidities are the same with the laparoscopic approach. Hernias, wound infections, and stomal stenosis problems may be less common with the laparoscopic approach. There may be a slightly higher rate of leak after the laparoscopic gastric bypass (see below under complications). At Washington University, we have offered the laparoscopic approach to selected individuals since April 1999 and our results confirm that this is a safe alternative.
Beneficial Outcomes
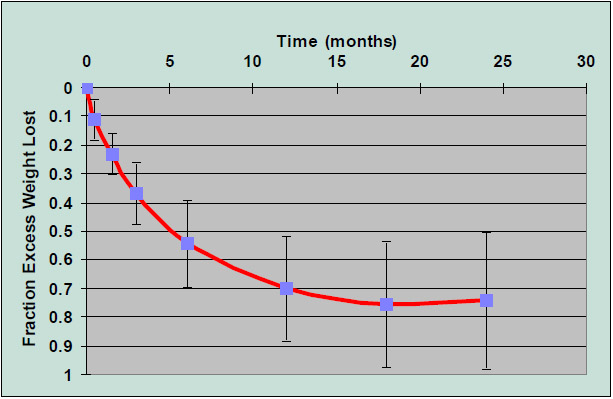
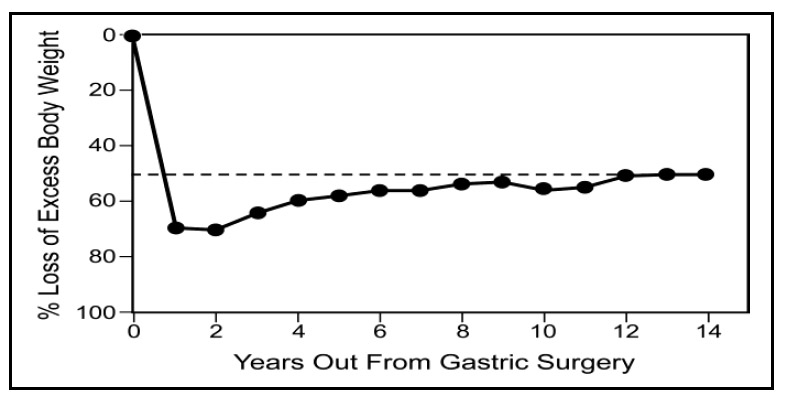
After gastric bypass, patients can expect to lose 70% of their excess body weight within a one to two year time span (figure 2). Those with a BMI over 55 will likely lose more pounds but a smaller percentage of their excess weight compared to those with a BMI under 55. Weight is lost most rapidly in the first few weeks and months with half of the weight loss occurring in the first three to four months. Long-term studies with high rates of follow-up have shown excellent long-term weight stability. There is on average slow weight gain after the first one to two years, but patientsmaintain loss of 50% of initial excess weight up to at least 15 years after surgery (figure 3). Figure 2: Fraction ofExcess Weight Lost after Roux Y Gastric Bypass at Washington University Figure 3: Long term weight loss results after gastric bypass: From Pories, et al, 1994.
Although the effect of surgery on weight is dramatic, the majority of patients ultimately plateau at a weight where they are classified as obese or overweight. The most compelling reason to argue in favor of surgical treatment of obesity is the dramatic improvements in obesity related co-morbidities. Over two thirds of patients being treated for diabetes will have normalization of their blood sugars and come off of all diabetic medication, essentially cured of their diabetes. Obese patients who do not have diabetes at the time of surgery have reduced incidence of developing diabetes by a factor of 30 compared to patients who do not have surgery. One half of the patients being treated for high blood pressure will be able to come off their blood pressure medication in the years after surgery, and a quarterwill have reduction in their dosages. It also reduces the risk of new onset high blood pressure by a factor of 10
compared to those not having surgery. Finally, those patients suffering from sleep apnea or other respiratory disturbances related to obesity will have dramatic improvements in their sleep quality, and 80% of those treated withCPAP are able to come off of that treatment.
Many of these co-morbidities directly affect the risk of heart disease. There is evidence that surgical treatment improves the chances of long-term survival in obese patients compound to those who do not have surgery. In diabetic obese patients, surgery reduced the risk of dying by a factor of five compared to those who were eligible for surgery but did not receive it because they were turned down or were denied authorization by their insurance company.
As with all surgical procedures, risk is involved. This is a major surgical procedure performed on patients who in general are not a healthy group. Our average patient has two co-morbidities in addition to their obesity. Obesity itself is associated with increased risks of surgery. Approximately 30% of our patients will suffer some form of complication, although the vast majority is minor. It is important that you understand the potential risks.
The following table describes the frequency of various complications at Washington University from July 1997 through May 2008.
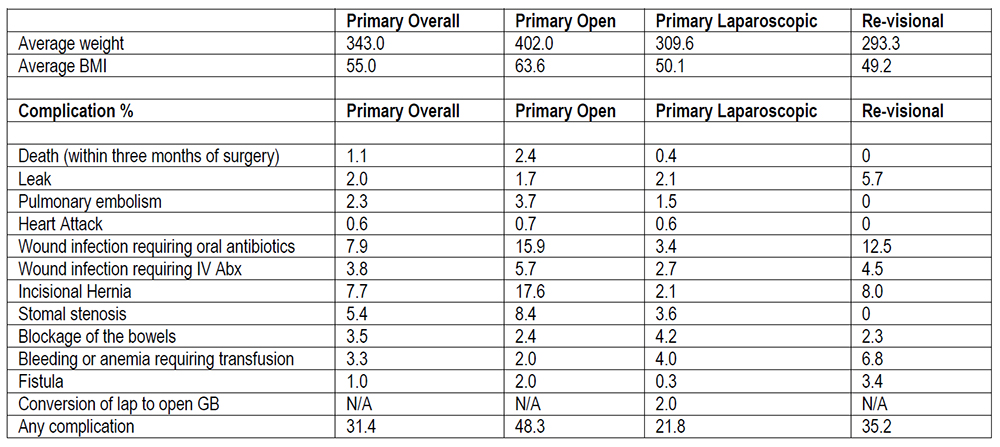
Death. Among all patients who have gastric bypass, 1-2% die within three months of surgery. The three most common causes of death are heart attack, pulmonary embolism (blood clot going to the lungs), and a leak at the connection of the stomach and the small intestine. The risk of death seems to be higher in heavier patients and those patients who have severe respiratory problems associated with their obesity, but even patients with no co-morbidities have died from this operation. It is not possible to accurately predict who will die from surgery, and you must be willing to accept this risk, or you should not have surgery.
Leak. One of most serious complications is a leak from an anastomosis or hook up. This can cause a serious condition known as peritonitis and result in the formation of pockets of infection called abscesses. Leak is rare (2-4%) and can be minor, but it can be extremely serious and potentially fatal. Leaks typically occur in the first few days to a week after surgery. All patients are checked for leaks 5-10 days after surgery with an upper GI test. If a leak occurs, emergency surgery may be necessary. Leaks are around 2 – 3 times as common when gastric bypass is done as a revision of previous gastric obesity surgery.
Heart Attack. Risk is low but increases with age, smoking and number of co-morbidities.
Blood clots. As with other types of surgery blood clots can form. These typically form in the blood vessels of the arms and legs and can break off and flow to the lungs where they may block the flow of blood to the lung- a pulmonary embolism. You will be given a blood thinner called heparin before and after surgery, and special boots will be placed on your feet to help pump blood back from the veins in your legs to your heart. Even with all these precautions, it is not possible to completely eliminate the risk of blood clots.
Stenosis. The opening formed by the attachment of the intestine to the stomach pouch may become smaller as healing occurs in the first 4-8 weeks. This is known as stenosis. As a result, solid food cannot pass through the opening, resulting in severe nausea and vomiting after eating. If this occurs, the opening can be enlarged to its original size by passing a tube called an endoscope into the stomach and stretching the opening with a small balloon.
Hernia. A hernia occurs when the muscle wall that normally covers the stomach and intestine becomes weakened at the point at which it was sewn together. A small sac-like pocket forms under the skin. The intestines can enter this pocket, where they can become trapped. Surgical repair is eventually necessary.
Ulcer. Gastric bypass surgery increases the chance that you will develop an ulcer during your lifetime. This is almost always treatable with medications. To help prevent this, antacid medication (Pepcid) must be taken daily for one month following surgery to help prevent this complication.
Gallstones. During the period of rapid weight loss, individuals who have not had their gallbladder removed have a higher risk of developing gallstones. Medication is prescribed (Actigall) that must be taken daily for six months following surgery.
Fistula. In rare patients, the two compartments of the stomach separated at the time of the gastric bypass can reconnect. This may occur suddenly even years out from surgery and is associated with sudden dramatic weight gain and increased ability to eat.
Nutrient deficiencies and anemia. These are the most common long-term side effects of surgery, but they are generally avoidable. Because of the bypass of the lower stomach and upper small intestine, you will not absorb folic acid, vitamin B12, calcium and iron normally after surgery. It is critical that you continue to take a daily multivitamin, vitamin B12 and calcium every day for the rest of your life. Menstruating females will need to take daily iron supplements as well. Failure to take these, supplements can result in anemia and osteoporosis (brittle bones).
Overview of the evaluation
You will be spending time with members of the Washington University Weight Management Program including a behavioral counselor, dietitian, obesity surgeon and a physical therapist. During your visit with the surgeon, a thorough history will be taken. You will spend time with a dietitian, who will evaluate your eating habits and medical history. All of the evaluations will be used to assess you as a surgical candidate. You may be asked to do further testing to evaluate any potential obesity related problems such as sleep apnea and GE reflux disease. If so, the tests will be ordered by the surgeon. If you are an appropriate candidate for surgery a letter will be written to your insurance company requesting approval for the procedure. Expect about a one to two month wait between your initial visit and precertification and another one to two months until your scheduled surgery date.
Your role in Gastric Bypass Surgery
Most of our patients have been very pleased with the results of their operation. On average, patients have lost 70% of their excess weight after one year. Gastric bypass surgery is designed to help you help yourself. Individuals considering gastric bypass surgery must be committed to certain lifestyle changes in order to help insure healthy and successful weight loss and management. The success of the surgery depends on you. The surgery can be beaten; therefore, you must follow a few simple principles:
Eating style. Due to the reduced size of the stomach, food must be eaten slowly, in small portions and chewed well, otherwise nausea and vomiting can result. Eating larger portions can also eventually stretch the stomach, defeating the purpose of surgery. YOU MUST TAKE VITAMINS FOR THE REST OF YOUR LIFE.
Food choices. Eating foods that are high in dry fat calories, such as snack chips or fried foods will result in suboptimal weight loss as well as nutritional deficiencies. “NO JUNK FOOD” This is considered poison to a gastric bypass patient. This includes chips, crackers and buttered popcorn. “NO FRIED FOODS!” This includes french fries, fried fish and fried chicken. “NO SWEETS!” Foods such as regular soda, milk shakes, candy, cake and ice cream will likely result in lightheadedness, dizziness, sweating, nausea, abdominal cramping and diarrhea, i.e. dumping syndrome. If you test the system, you will likely be sorry you did.